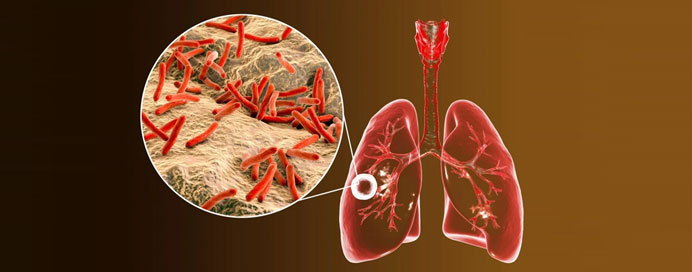
The treatment of tuberculosis (TB) involves a combination of medications to cure the infection and prevent the development of drug-resistant strains of the bacteria. TB is caused by Mycobacterium tuberculosis, and the standard treatment involves a regimen of antibiotics that must be taken for an extended period to ensure complete eradication of the bacteria. Treatment for TB is typically divided into two phases: the initial phase and the continuation phase. It's crucial to follow the prescribed treatment plan diligently and complete the entire course of antibiotics to prevent recurrence and the development of drug resistance.
1. Initial Phase (Intensive Phase):During this phase, the primary goal is to rapidly reduce the bacterial load. The most common medications used in the initial phase include:
The duration of the initial phase varies but typically lasts for 2 months. In some cases, if the TB strain is found to be susceptible to all drugs and the patient is responding well, the initial phase may be shorter.
2. Continuation Phase:The continuation phase typically lasts for 4 to 7 months, depending on the specific regimen and the patient's response to treatment. In total, TB treatment usually lasts for 6 to 9 months.
3. Directly Observed Therapy (DOT):DOT is a recommended strategy for ensuring that patients adhere to their TB medication regimen. It involves a healthcare provider or another trained individual directly observing the patient taking their medication. This helps to prevent treatment non-compliance and the development of drug resistance.
4. Drug-Resistant TB:In cases of drug-resistant TB, which may result from improper treatment or previous exposure to TB medications, treatment becomes more complex. Drug-resistant TB may require a longer course of treatment with second-line drugs that are less effective and often more toxic. Multidrug-resistant TB (MDR-TB) and extensively drug-resistant TB (XDR-TB) are more challenging to treat and may require treatment for up to two years or longer.
5. Monitoring and Follow-Up:Patients receiving TB treatment should be monitored regularly by healthcare providers to assess their progress, manage side effects, and ensure treatment adherence. It's essential to report any side effects or concerns to your healthcare provider promptly.
6. Infection Control:TB is highly contagious, and individuals with active TB should take precautions to prevent the spread of the disease to others. This includes wearing a mask, practicing good respiratory hygiene, and avoiding close contact with others, especially in enclosed spaces.
TB treatment can be effective when taken as prescribed, and it is essential to complete the entire course of antibiotics to prevent relapse and drug resistance. Failure to complete treatment or non-compliance with the prescribed regimen can lead to more severe drug-resistant forms of TB, which are more challenging and expensive to treat. Therefore, it is crucial to work closely with healthcare providers and follow their recommendations throughout the treatment process.